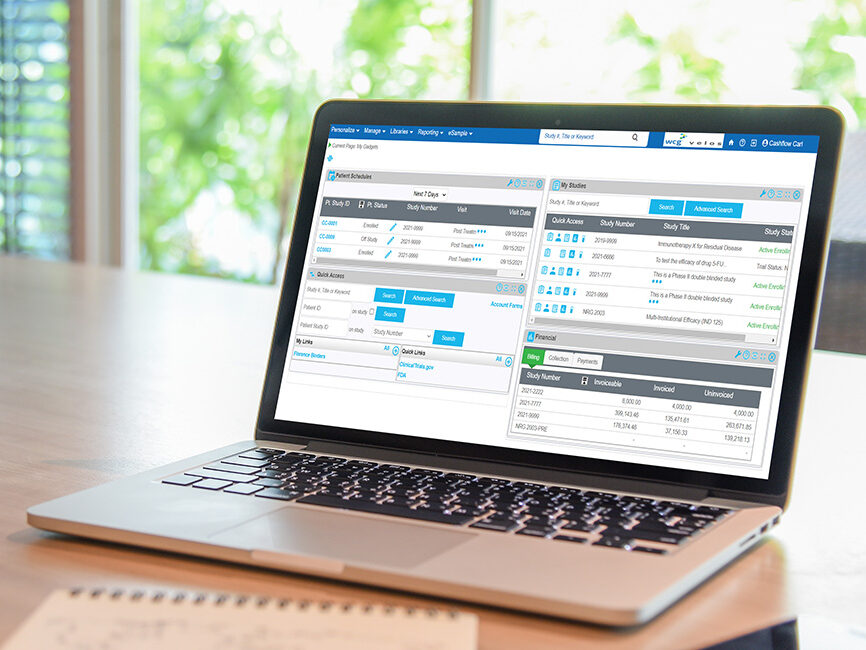
eResearch CTMS
An integrated platform designed to support all of your site’s clinical trials and research activities, from start-up through close-out.
Operational efficiency and consistency. Financial oversight. Interoperability across technologies. In today’s complicated clinical research environment, sites need increased financial visibility and strong operational oversight in addition to increased coordinator and participant support.
WCG eResearch CTMS is a comprehensive and adaptable clinical trial management system designed to automate all administrative, financial, and research activities to help sites accelerate their research management with scalable growth and continuous improvement.
Our clients – including academic medical centers, hospitals, health systems, and independent sites – tell us they are more productive and efficient with WCG eResearch CTMS.
WCG eResearch CTMS Supports Your Clinical Research Site With:
Integrated operations
Connect across technologies to provide information and reporting insights, enhance visibility within the organization, and increase end-to-end operational efficiency and consistency.
Financial and regulatory oversight
Efficiently evaluate study opportunities, ensuring fast turnaround for customer satisfaction and sponsor payment, while meeting compliance standards to manage risk, avoid penalties, and support audits.
Coordinator and participant-centricity
Effectively manage participants and visits with the included participant portal for remote participant engagement and self-reporting. Oversee numerous studies simultaneously while eliminating duplicate data entry and the need to interface with multiple, complex systems.
Real Results with WCG eResearch
WCG eResearch CTMS helps you ensure a single source of truth for coordinators as they access study documents and interface with EHRs and other enterprise systems. Your team will spend less time on administrative work and more time with participants, using our intuitive and dependable technology.
reduction in time spent on data entry
improvement in site financial results
system integrations, including 50+ with Epic
increase in participant retention rates
Customer Stories
Simplifying Clinical Research Processes Across a Large Academic Medical Center with WCG eResearch
- Improved financial transparency with coverage analysis documentation, calendar, budget, and milestone entry.
- Demonstrated increased efficiency and profitability with the integrated tracking of account receivables and invoices.
- Eliminated duplicate data sets across multiple departments.
There’s rarely a question we can’t answer with WCG. WCG eResearch has improved our institution’s research programs and operations, and as a result, improved the attractiveness of our site to sponsors and CROs.
– Director of Research Information Management, Large Academic Medical Center
Part of an Integrated Research Platform
WCG eSample
Manage all biospecimens for your research, or set up biobanks or biorepositories using one secure platform.
WCG eSample enables biobanks, biorepositories, and research sites to manage specimens of all types on one secure, centralized, and integrated platform.
WCG Participant Portal
Engage participants and facilitate research in remote settings.
WCG Participant Portal is designed to sustain and accelerate research even in remote settings, encouraging compliance and timely communication between participants and care providers.
WCG eResearch CTMS FAQs
Q: What will happen to studies and participants that we have been managing in spreadsheets or other systems?
We understand the importance of legacy data on spreadsheets or in other systems. Rather than starting your clinical trial program from ground zero, you get access to your existing data with our professional services. Data migration is accurate and efficient, and we position you for successful implementation and product adoption.
Q: Can WCG eResearch CTMS be connected to my EMR and other systems?
Yes. Sites that want to develop integrated ecosystems turn to us because we have an open platform with extensive APIs. EMR integrations include ADT for demographics, RPE for protocol and subject information exchange, and IHE CRPC billing designations to ensure billing compliance. In addition, we offer standard and custom integrations with other third-party systems such as IRB platforms, financial, clinical and regulatory systems, etc.
Q: How can sites ensure data privacy and compliance?
WCG maintains an extensive Privacy Policy and portfolio of SOPs supporting it that cover privacy by design, data privacy impact assessments, data rights requests, etc. Our privacy policy can be found at www.wcgclinical.com/privacy-policy. WCG eResearch incorporates capabilities to help enforce 21 CFR Part 11 and HIPAA compliance.
Q: What are the different hosting options available to sites?
We provide secure cloud-hosted infrastructure to alleviate the security, maintenance and licensing burden on sites. We also offer an on-premises hosting option.
Schedule a demo of WCG eResearch CTMS
Learn how you can streamline your clinical trials and improve productivity. By completing this form, someone will reach out to you within 24 hours to set up a demo of our industry-leading CTMS technology.
Recent Insights

7 Key Considerations for Research Sites Contemplating Switching Their CTMS
Blog Posts
Clinical Trial Technologies for Sites: Building an Innovative Clinical Trial Technology Roadmap For Your Research Program
Videos